Dementia is the loss of cognitive functioning – thinking, remembering, and reasoning – and behavioural abilities to such an extent that it interferes with a person’s daily life and activities.
Alzheimer’s disease, the most common form of dementia and the focus of the research at Bournemouth University, results in declines in navigation skills that are accentuated in unfamiliar environments. Many people with Alzheimer’s eventually face the challenge of having to learn their way around new environments, such as a care home. People with Alzheimer’s disease would have an easier transition moving to new residences if these environments were designed for decreasing orientation skills.
Creating ‘dementia friendly’ guidelines
Few existing ‘dementia friendly’ design guidelines specifically address navigation and orientation issues. Those that do are currently not well integrated with psychological knowledge, navigation research or the views of residents.
Under the guidance of BU Professor of Psychology Jan Wiener, Mary O’Malley, a BU PhD student, has been exploring how people with dementia learn to navigate unfamiliar environments and what consequences this could have for dementia care home building and design guidelines.
A positive impact on people with dementia
To date, Mary’s five years of research, in conjunction with the ARDC (The Ageing and Dementia Centre) at BU, has resulted in the creation of ‘dementia friendly’ design recommendations. These are based on psychological evidence and the views of people with dementia, and are widely applicable to architects, building standards agencies, care commissioning bodies and practitioners.
The overall aim is that the recommendations will be used to develop national design standards for residential care homes – and one of the homes where she carried out her research is now intending to have a full re-design. Mary is also aiming to extend her research to other public places, such as hotels, shops and hospitals, to help those with dementia with their navigation and way finding.
*Source: Alzheimer’s Research UK

Professor Jan Wiener
Our research has very real implications for the design of care homes and other public places. It provides an evidence base for building guidelines, based on what our research shows helps and hinders people to navigate environments
A new, psychological approach
Building on his years of research into navigation and wayfinding, in 2017 Professor Wiener obtained funding from the Economic & Social Research Council (ESRC). This enabled ongoing research into how people with dementia navigate around different environments and what hinders them.
Led by Mary O’Malley, the Dementia and Wayfinding project has focused on gaining a psychological understanding of which aspects of care home living are used in orientation and navigation. Mary also spoke directly to people with dementia to understand how they find their way within a care home setting and to understand their design preferences. Residents’ design suggestions focused heavily on the importance of having memorable and meaningful spaces which were favoured more than signage as an orientation aid.
Alongside speaking to people with dementia, Mary utilised the state-of-the-art technology in the BU Psychology Wayfinding Lab, including the creation of virtual care home environments, which allowed for variables – such as corridor layout and where landmarks are placed – to be changed. This was combined with eye tracker technology, which allows the team at BU to see exactly where people are looking and which waypoints they’re likely to use to help them get around.
Recommendations for enhancing navigation and orientation
In 2018, Mary spoke at a TEDx event on creating dementia friendly spaces, highlighting five recommendations.
Watch BU’s Mary O’Malley’s talk on creating dementia friendly spaces
Mary O’Malley’s research puts forward the following design principles for improving navigation and orientation in care home settings:
- Avoid having repetitive layouts and interior finishes
Repetitive layouts within a care home setting, such as similar pictures along the corridors, a lack of memorable spaces and limited colour contrast in carpets, can make it hard for people with dementia to learn and memorise new routes. These can impact on every day, simple tasks such as going to a communal lounge. - Landmarks
One way of breaking up repetitive spaces is to have enough memorable landmarks along the corridors of care home settings. A landmark, which is unique, memorable and salient acts a good tool for improving residents’ navigation. - Using colour effectively
Using different colours within the design of a care home setting can act as a distinct way to both break up and connect spaces together. Mary focuses on the importance of colour contrast and how, for example, too little colour contrast between furnishings such as carpets, walls and sofas may cause a resident to walk into these – whereas too much contrast, between flooring and a rug for example, could be perceived as a ‘hole’, causing distress to residents. - Reducing background noise
People with dementia can experience changes to their senses, including a sensitivity to noise. In her talk, Mary speaks about how to absorb noise with more soft furnishings in settings such as care homes. She also speaks about how noise can be accentuated through items such as monitors, radios and TVs, and where possible, to minimise this noise. - Good access to toilets and signage
Mary’s final recommendation tackles an issue which has rarely been discussed in previous research into the navigation of people with dementia – ensuring not only good access to toilets, but also that people are easily able to navigate their ways to and from the bathroom. In addition, Mary talks about how signage to and from toilets in public spaces can be minimal along with the use of colour contrast to differentiate different areas of bathrooms (such as soap dispensers, floors and walls).
Mary O’Malley
Bournemouth University, during her TEDx talk
By changing people’s perceptions of what dementia is, this will create a more user friendly and accessible environment that will not only benefit those with dementia but will benefit the community as a whole.
Where it all started
Professor Wiener’s dedicated years of research into navigation and orientation, which uses approaches such as virtual reality techniques and eye-tracking, has been applied directly into two public settings.
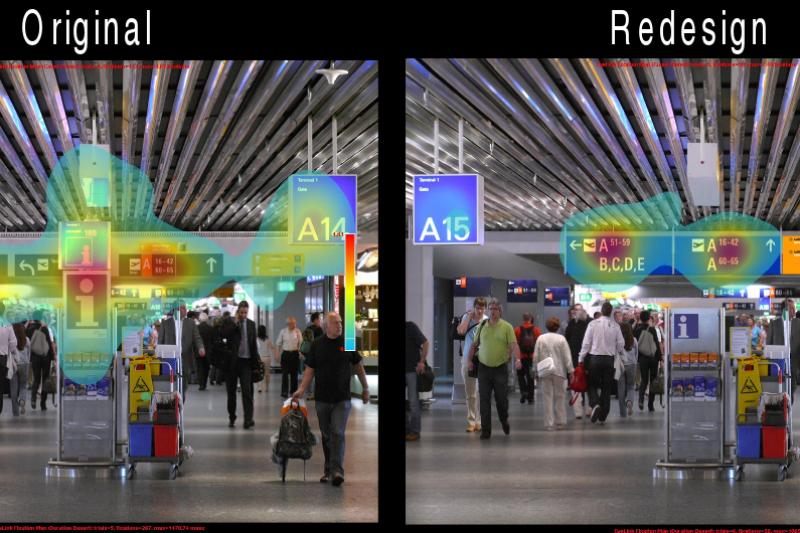
The first was at Frankfurt Airport in 2012, where in collaboration with the Centre for Cognitive Science in Germany, the signage at a number of key transfer locations was changed to improve the flow of airport ‘traffic’ when navigating gate routes.
The redesign had a positive effect on passengers’ wayfinding behaviour, including an increase in their response time to the new signage when utilising the eye-tracking technology.
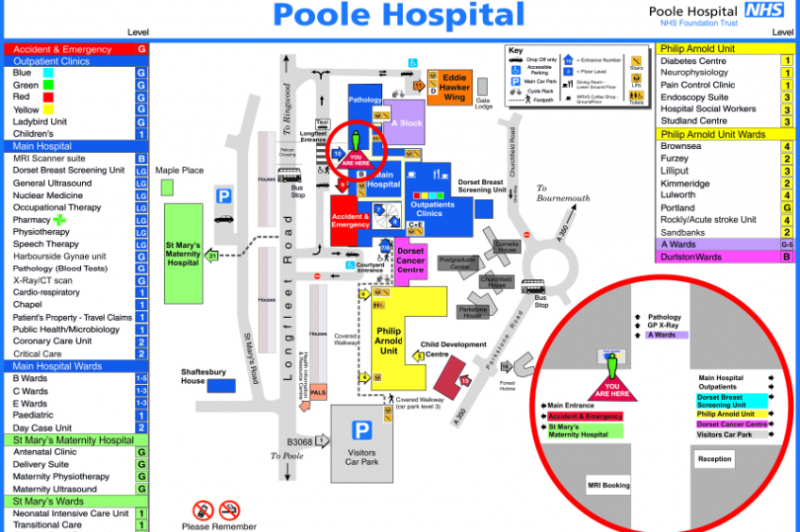
Following the success of the improvements to signage in Frankfurt, in 2013, the BU Wayfinding Research Group, led by Professor Wiener, was commissioned by Poole Hospital in Dorset to help improve visitor wayfinding.
After analysing the existing maps, the BU team changed several aspects, including adding a ‘You Are Here’ symbol. From this, 98% of people could plan correct routes to a chosen destination – an almost two-fold increase in accuracy. Furthermore, visitors were able to decide on their routes more quickly with the new maps – in fact, they were 37% faster.
Most recently in 2018, Professor Wiener and the BU ADRC team launched the new SAT NAV education programme (SustAining residenT NAVigation in care environments), where alongside 28 practitioners – including care home managers, architects, and interior designers – they are developing further plans and rollouts to support people with dementia in unfamiliar environments. This builds on the research of Mary O’Malley.
The Alzheimer’s Society forecasts that the number of people living with dementia in the UK will increase to over 1 million by 2025 and over 2 million by 2051. This makes research and innovations in this area vital – and the ongoing work of the ADRC is playing an important role in helping to tackle some of the challenges faced by those affected by dementia, their families, and healthcare workers.